Recognizing Pulmonary Embolism Symptoms: A Guide to Early Detection and Care
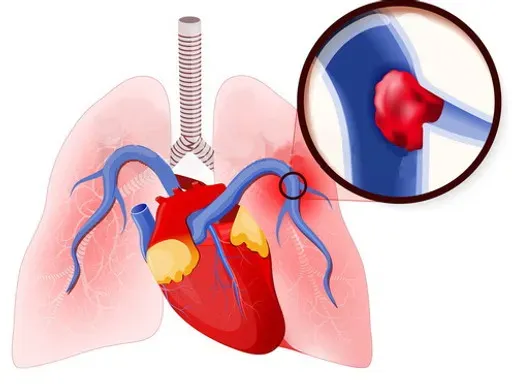
Pulmonary embolism (PE) is a serious medical condition caused by a blockage in one of the pulmonary arteries in the lungs, most often due to blood clots. Timely recognition of its symptoms is crucial to ensuring effective treatment and reducing the risk of life-threatening complications. In this article, we explore the symptoms, potential causes, risk factors, and when to seek medical attention for pulmonary embolism.
What is Pulmonary Embolism?
Pulmonary embolism occurs when a blood clot, usually formed in the deep veins of the legs (a condition known as deep vein thrombosis or DVT), travels to the lungs and blocks blood flow. This condition can compromise oxygen delivery throughout the body, making it a medical emergency.
Key Pulmonary Embolism Symptoms
Recognizing the symptoms of pulmonary embolism can be challenging, as they often mimic other conditions. However, understanding the common signs is essential:
- Shortness of Breath
- Sudden and unexplained breathlessness is one of the hallmark symptoms of pulmonary embolism. It can occur during rest or physical activity.
- Chest Pain
- Sharp or stabbing pain that worsens with deep breathing, coughing, or physical exertion may indicate a pulmonary embolism.
- Coughing
- Persistent coughing, sometimes accompanied by blood-tinged mucus, can signal a blockage in the pulmonary artery.
- Rapid Heart Rate
- A racing or irregular heartbeat is often the body’s response to reduced oxygen levels caused by the embolism.
- Lightheadedness or Dizziness
- A sudden feeling of faintness, dizziness, or even loss of consciousness can be a sign of a significant clot.
- Swelling or Pain in the Legs
- Often linked to DVT, swelling, redness, or tenderness in one or both legs might indicate a clot that could lead to pulmonary embolism.
- Bluish Skin Tone (Cyanosis)
- A bluish tint to the skin, particularly around the lips or fingertips, occurs due to reduced oxygen in the blood.
Understanding the Risk Factors
Certain factors increase the likelihood of developing pulmonary embolism:
- Prolonged Immobility
- Sitting for extended periods, such as during long flights or hospital stays, can slow blood flow in the legs, leading to clots.
- Surgery or Injury
- Recent surgeries, particularly orthopedic ones, and severe injuries can elevate the risk of clot formation.
- Chronic Conditions
- Heart disease, cancer, and inflammatory conditions like lupus heighten the risk.
- Lifestyle Factors
- Smoking, obesity, and lack of physical activity can contribute to blood clot development.
- Hormonal Influence
- Pregnancy, oral contraceptives, and hormone replacement therapy can increase clotting potential.
- Genetic Predisposition
- A family history of blood clots or inherited clotting disorders may put individuals at risk.
When to Seek Medical Help
Pulmonary embolism is a medical emergency that requires immediate attention. Seek medical help if you or someone you know experiences:
- Severe shortness of breath.
- Intense chest pain.
- Persistent coughing with blood.
- Symptoms of shock, such as rapid heart rate, sweating, and confusion.
Prompt diagnosis through imaging tests like CT scans, pulmonary angiography, or ultrasound (for DVT detection) can save lives.
Prevention Tips
While not all cases of pulmonary embolism are preventable, adopting the following strategies can lower the risk:
- Stay Active
- Avoid sitting for long periods. If traveling, take regular breaks to stretch and move around.
- Use Compression Stockings
- These can help improve blood flow in the legs, particularly after surgery or during prolonged immobility.
- Follow Medical Advice
- Adhere to prescribed anticoagulant medications if you are at high risk.
- Maintain a Healthy Lifestyle
- Regular exercise, a balanced diet, and quitting smoking are crucial for overall cardiovascular health.
- Hydrate Properly
- Dehydration can contribute to blood thickening, so drink plenty of water, especially during long journeys.
Treatment Options
Once diagnosed, treatment for pulmonary embolism focuses on dissolving the clot and preventing new ones from forming:
- Anticoagulants (Blood Thinners): These prevent further clot formation and allow the body to break down existing clots.
- Thrombolytics (Clot Busters): Used in severe cases, these medications quickly dissolve clots.
- Surgical Intervention: In critical situations, procedures like catheter-directed thrombolysis or embolectomy may be necessary.
- Oxygen Therapy: This helps maintain adequate oxygen levels in the blood.
Living with Pulmonary Embolism
If you have experienced a pulmonary embolism, follow your healthcare provider’s advice to prevent recurrence:
- Attend regular follow-ups.
- Take prescribed medications as directed.
- Be proactive about recognizing symptoms early.
Conclusion
Understanding pulmonary embolism symptoms is essential for early diagnosis and timely treatment. Educating yourself about risk factors and prevention strategies can reduce your chances of experiencing this life-threatening condition. If you or someone around you shows symptoms, don’t hesitate to seek medical help immediately—it could save a life.
By staying informed and vigilant, we can work towards a healthier and safer future.






